Welcome to the educational program Managing Difficult Behaviors. This program will present some principles and strategies for preventing and managing difficult behaviors.
. . .
This is Lesson 17 of The Alzheimer’s Caregiver. You may view the topics in order as presented, or click on any topic listed in the main menu to be taken to that section.
We hope that you enjoy this program and find it useful in helping both yourself and those you care for. There are no easy answers when it comes to the care of another, as every situation and person is different. In addition, every caregiver comes with different experiences, skills, and attitudes about caregiving. Our hope is to offer you useful information and guidelines for caring for someone with dementia, but these guidelines will need to be adjusted to suit your own individual needs. Remember that your life experiences, your compassion and your inventiveness will go a long way toward enabling you to provide quality care.
Let’s get started.
Prefer to listen to this lesson instead? Click the Play button on the playlist below to begin.
Types of Difficult Behavior
Difficult behaviors can be categorized as verbally nonaggressive, verbally aggressive, physically nonaggressive, and physically aggressive.
Examples of verbally nonaggressive behaviors include complaining,  negativism, repetitive questions, and constant requests for help. Verbally aggressive behaviors include cursing, making distressed noises, verbal sexual advances, and screaming. Examples of physically nonaggressive behaviors are disrobing, eating inappropriate things, handling or moving items, wandering, hoarding, and hiding. Lastly, and perhaps most concerning, are physically aggressive behaviors such as physical sexual advances, hurting self or others, throwing items, grabbing, pushing, hitting, spitting, kicking, and biting.
negativism, repetitive questions, and constant requests for help. Verbally aggressive behaviors include cursing, making distressed noises, verbal sexual advances, and screaming. Examples of physically nonaggressive behaviors are disrobing, eating inappropriate things, handling or moving items, wandering, hoarding, and hiding. Lastly, and perhaps most concerning, are physically aggressive behaviors such as physical sexual advances, hurting self or others, throwing items, grabbing, pushing, hitting, spitting, kicking, and biting.
When a difficult behavior occurs, caregivers should ask themselves a key question: “Is there a need or reason that explains the behavior even if not apparent to the observer?” An important concept is that all behavior has meaning, and it is the caregiver’s responsibility to figure out that meaning. What is the person trying to communicate with the behavior? Possible needs and reasons include pain, distress, fatigue, thirst, hunger, toileting needs, constipation, fever, medication issue, and infection or other medical issue. The caregiver should try to address these needs before difficult behaviors occur or before difficult behaviors escalate.
Another important concept is that the person is not intentionally being difficult. It is the disease, not the person, causing the behavior. The behavior may be the only way that the person knows of communicating feelings, needs, or wants. The person may not appreciate that the behavior is inappropriate and may need a gentle reminder about what is acceptable behavior. But do not blame or reproach the person for the behavior. The challenge is to find out what triggered the behavior and to intervene accordingly.
Management Guidelines
Difficult behaviors can successfully be managed while providing the person with dementia quality of life. There a few guidelines that can help ensure success.
First, identify specific problem behaviors and design specific interventions.
Set appropriate and realistic goals. Even small improvements in behavior should be considered successes.
Reassess and adjust as needed. Make ongoing assessments of behaviors and the effectiveness of strategies. Try adjusting approaches or come up with new, creative ways of managing behaviors.
Be willing to try many things. Consider modifying environments, care routines, activities, diet, family involvement, and in care facilities, staff training programs.
Consider using a combination of medication and behavior approaches. Sometimes a combination of approaches is most effective. But in all cases, non-pharmacological approaches should be attempted.
The best dementia care approaches use flexible problem-solving to prevent problems before they occur. Oftentimes, difficult behaviors occur because needs are not met. Therefore it is important to anticipate needs and address them before difficult behaviors occur.
Caregivers can determine how best to serve their care recipients by knowing about each individual’s life story, preferences, and abilities. Good dementia care uses information about those with dementia to develop “person-centered” strategies to meet their needs. Keep in mind that for people with dementia, quality of life depends largely upon the quality of the relationships they have with caregivers.
Some key principles for managing difficult behaviors include reducing frustration and fear, providing safety, security, and comfort, and using good communication techniques. We will discuss each of these principles in more detail.
Person-Centered Care
The underlying premise of this program on managing behaviors is that using person-centered care when assisting with any activity will go a long way towards preventing difficult behaviors. What do we mean by person-centered care?
 Person-centered care means to individualize the care to the person’s wants, needs and values, rather than that of the caregiver or facility. It takes into consideration the person’s past life experiences and roles, preferred habits and routines, cultural norms, expectations, and spiritual preferences, and builds upon the person’s retained skills and capacities.
Person-centered care means to individualize the care to the person’s wants, needs and values, rather than that of the caregiver or facility. It takes into consideration the person’s past life experiences and roles, preferred habits and routines, cultural norms, expectations, and spiritual preferences, and builds upon the person’s retained skills and capacities.
Another key principle in managing difficult behaviors is the use of validation. Validation promotes the belief that each and every individual has value. It is helpful to know the person’s life history and to use information from that history to show that she or he is important. Caregivers can help care recipients reminisce about people and events and validate lifelong beliefs and identities. It is important to use empathy to build trust, reduce anxiety and promote dignity.
To learn more about person-centered care, please see the LightBridge library of products.
Case Study 1
Let’s look at a situation with Robert, who has Alzheimer’s disease, and Sally, his at-home nurse. Robert has recently been getting upset about Sally having to help him bathe, because his wife Mary can no longer lift him by herself. Sally must do her best to prevent any agitation or difficult behavior during bath time.
Sally begins by prepping the bathing area and looks around to see if there is anything that may appear threatening to Robert. She knows that mirrors can confuse or frighten Robert so she covers it.
Sally also knows that Robert enjoys country music and tends to get cold coming out of the shower so she turns on his music and warms up the room. She also makes sure that the lavender oil scent fills the room as she knows that it helps to relax him.
Sally knows that Robert is frightened, so she only looks at him in the eyes and uses reassuring words. She also encourages him to do as much as he can for himself during all activities.
Frustration and Fear
An important strategy for preventing difficult behaviors is to reduce the person’s frustration and fear.
 In the video, Sally was careful to engage with both Mary and Robert. The key points are that she made the activity a pleasant, social occasion supportive of both persons using her attitude and communication skills. She reduced the risk of sensory overload by reducing clutter and removing objects that might cause fear or confusion. She added the soothing sound of Robert’s favorite music, because music has been shown to be an effective approach of reducing agitation behaviors. Lastly, she made sure the scent of lavender filled the room, because she knows that aromatherapy can help reduce his anxiety. Sally is aware that aromatherapy using lavender or essential oil of lemon balm applied to the face and arms can reduce agitated behaviors in people with dementia.
In the video, Sally was careful to engage with both Mary and Robert. The key points are that she made the activity a pleasant, social occasion supportive of both persons using her attitude and communication skills. She reduced the risk of sensory overload by reducing clutter and removing objects that might cause fear or confusion. She added the soothing sound of Robert’s favorite music, because music has been shown to be an effective approach of reducing agitation behaviors. Lastly, she made sure the scent of lavender filled the room, because she knows that aromatherapy can help reduce his anxiety. Sally is aware that aromatherapy using lavender or essential oil of lemon balm applied to the face and arms can reduce agitated behaviors in people with dementia.
All strategies that concern reducing fear and frustration are most successful when the caregiver knows the person’s history.
First, get to know people and what might trigger their fear or frustration. This will help you to appreciate and understand their sensitivities and reactions, and to respond to them as individuals with approaches that work best with them.
Second, observe behavior and other non-verbal messages to know their mood and levels of stress and anxiety.
Third, simplify and slow down all activities. Appreciate the moment! Be sure to engage the person. Sit next to them, get close, smile, speak their name and make eye contact. Use gentle directing during tasks and gently redirect the person if their attention wanders. Always remember to be calm yourself, and you will convey calmness and trust.
Safety, Security, and Comfort
Because people with dementia have such difficulty comprehending their environment, it is important to provide a safe, secure, and comfortable setting, taking into consideration both the physical and human environments. A safe physical setting includes being safe from walking out a door and becoming lost or injured in traffic; safe from injuries such as burns from steam or hot water; safe from handling or ingesting poisons; safe from falls resulting from clutter, uneven walkways or slippery floors, and safe from sharp objects that could cause cuts. A safe human  environment includes being safe from physical or emotional abuse from untrained or poorly motivated caregivers, and safe with regard to medical care and medication administration.
environment includes being safe from physical or emotional abuse from untrained or poorly motivated caregivers, and safe with regard to medical care and medication administration.
Feeling secure in the physical and human environments is also a priority. People with Alzheimer’s have less ability to recognize people and places, and the environment can appear confusing and threatening. It is important to surround them with familiar people, objects, sounds, and smells, and to keep familiar routines. Playing preferred music and providing aromas using lavender or Melissa oil can help relax people. Providing calm and reassuring human support also promotes a sense of security. Try to minimize exposure to complex, noisy, or unfamiliar environments.
Comfort is another core principle in dementia care. Because those with dementia are less able to make their needs known, they may be hungry or thirsty but unable to ask for food or water. Or they may be fatigued or in pain without being able to express this. It is important to look for subtle signs of discomfort and to check frequently for needs such as food, drinks, pain management, or toileting. Caregivers should try to anticipate needs and meet them. If someone has a tendency to be incontinent, make frequent trips to the toilet with her or him, and make sure that clothes are clean and dry. Clothing should be comfortable, fit properly, reflect the weather and the occasion, and be easy to manage for dressing and undressing. Keep in mind that older people have trouble regulating their temperature and so may feel cold even when younger people feel warm. So offer layers of clothing and set the thermostat to ensure their comfort.
Safety, Security, and Comfort (Continued)
Part of providing a secure and comfortable environment includes showing love and respect for the person with dementia. There are many ways to  show love and respect, but the message should be genuine and provided in a way so that the person understands the message. Because many care activities involve physical contact, respect for a person’s privacy is sometimes neglected. Toileting, bathing and dressing interactions need to be conducted with respect for the individual’s privacy and modesty. If in a care facility, spouse or family visits should be encouraged and space provided for private accommodations. Though the disease does result in a reversal of functional abilities, meaning some behaviors become child-like, the person is an adult with a lifetime of contributions, and should be treated with dignity. Expressions of love and affection can include smiles, hand holding, hugs, and pats, keeping in mind that people respond to touch differently and are comfortable with different levels of affection. It is a good idea to use caution with touch until rapport and trust are established.
show love and respect, but the message should be genuine and provided in a way so that the person understands the message. Because many care activities involve physical contact, respect for a person’s privacy is sometimes neglected. Toileting, bathing and dressing interactions need to be conducted with respect for the individual’s privacy and modesty. If in a care facility, spouse or family visits should be encouraged and space provided for private accommodations. Though the disease does result in a reversal of functional abilities, meaning some behaviors become child-like, the person is an adult with a lifetime of contributions, and should be treated with dignity. Expressions of love and affection can include smiles, hand holding, hugs, and pats, keeping in mind that people respond to touch differently and are comfortable with different levels of affection. It is a good idea to use caution with touch until rapport and trust are established.
Being able to be independent, autonomous and in control of our own decisions are matters of pride for most of us. This is also true for persons with dementia, and these attributes should be encouraged.
Loss of independence often results in feelings of worthlessness, and as feelings of worthlessness increase, competence decreases. Therefore it is important to encourage as much self-care as possible and assist only as needed.
Until the very late stages of dementia, every effort should be made to support the person’s retained capacities. The dilemma is how to support independence while at the same time insuring physical safety. The key is to provide guidance at the individual’s level of abilities without taking over. For example, it is probably not safe for an 88-year-old man in the later stages of dementia to walk an uneven, rocky path to visit a favorite horse. If the visit will give him pleasure and memories of healthier times, he could be assisted or transported to the horse to make the visit possible. The choices and the activities need to reflect the level of the individual’s capacity to master them, but caregivers need to constantly monitor the line between safety and autonomy.
Using Communication
The way one communicates with someone with Alzheimer’s disease is very i mportant in managing difficult behaviors. How one says something is just as important as what is said.
mportant in managing difficult behaviors. How one says something is just as important as what is said.
People with Alzheimer’s disease have shorter attention spans and, because they are older, may also have hearing loss. To give the best message, what one says needs to be very clear and simple, using familiar language, and with only one message in a sentence. Using the important word last will help the person retain the message. For example: “Robert, it is time for your bath.”
There is a lot that is said just by the inflection and tone of one’s voice. There are dozens of ways to say something. For example, the simple phrase: “Robert, come with me,” can sound inviting, or it can sound rough, like a demand. Though persons with Alzheimer’s disease have lost much of their logical thought abilities, they often retain an uncanny sense of the emotional climate of their environment. They can sense the emotional tone others convey, whether it be hostility, fear, humor, or joy. Therefore using a relaxed, clear, low and pleasant tone of voice can help those with dementia to relax or calm down.
Even though you may not feel like it at times, projecting a pleasant or joyful attitude will be comforting to those with dementia and will make caregiving tasks easier.
Using Communication (Continued)
Verbal communication should be kept simple to prevent frustration or confusion. Present information in one or two phrases at a time. If you are directing someone to do a task, break down the instructions into simple steps. For example, if you are assisting someone to put on a jacket, say, “Robert, here is your jacket.” Then, “Put your arm through this sleeve. I will  wrap it around your shoulder.” Followed by, “Now put your arm through this other sleeve.” Then, “Now button the first button.” Pause, “Now button this button” … and so on until the task is done.
wrap it around your shoulder.” Followed by, “Now put your arm through this other sleeve.” Then, “Now button the first button.” Pause, “Now button this button” … and so on until the task is done.
Persons with dementia have difficulty taking in information, so simplifying the information and providing only small pieces at a time are less likely to cause confusion or stress. All communication, all activities, and all environments can be simplified and slowed down.
Another very useful technique is redirection or distraction. Because of the short attention span of those with dementia, it is often easy to change their focus by introducing a positive topic or activity, like reading or listening to music. Redirecting is especially helpful with behaviors such as arguing, fighting, and pacing.
Click here to learn more about communication techniques.
Non-Verbal Communication
Non-verbal communication or body language is just as important as if not more than verbal communication. This is because in the later stages of  Alzheimer’s disease, the capacity to understand words decreases but the capacity to understand body language usually persists. Children learn non-verbal messages from their parents before they understand words. They also communicate their needs non-verbally before they can say what they need. Because non-verbal skills are learned earlier, people with Alzheimer’s disease will retain those skills longer than verbal skills.
Alzheimer’s disease, the capacity to understand words decreases but the capacity to understand body language usually persists. Children learn non-verbal messages from their parents before they understand words. They also communicate their needs non-verbally before they can say what they need. Because non-verbal skills are learned earlier, people with Alzheimer’s disease will retain those skills longer than verbal skills.
Non-verbal communication includes facial expressions, body posture, and gestures. Keep in mind that the message that you give with your facial expression and other body language will override or cancel out what you are saying with your words. So make sure that your body language matches your words. If you are trying to calm someone down, use reassuring words with a smile, gentle tone of voice, and comforting gestures in a non-threatening posture.
Attending and Engaging
Some pointers that will help you to communicate with those with dementia are:
First, tune in to what they are trying to say, and be patient. If you listen carefully, you may be able to figure out what the person is trying to say even in the later stages of Alzheimer’s.
Second, respect their attempt to communicate even if facts and grammar are wrong. Do not try to correct them.
Third, avoid logical discussions and disagreements. Rather, try to make interactions pleasant and happy, and focus on the feelings and intent of the interaction.
If you are the one listening, don’t talk or interrupt. Listen attentively and show interest in what they are saying.
In a busy situation, it is so easy to hover over people, really not paying attention to them. In Alzheimer care, it is so important to truly engage with people when you are trying to find out what they need or to get them to do an activity. To engage means to get the individual’s attention by sitting and making eye contact. GET CLOSE so that they can see your face. Say the person’s name and wait for a response. If the person does not respond the first time, be patient and try again after a pause. Introduce yourself to the person. For example, say, “Robert. It’s Sally.” Pause for a response. Then say, “Robert, it’s time for your bath. Let me help you to the bathroom.”
If they do not understand you, they are more likely to be frightened or upset when you try to assist them to the bathroom. So check for signs of understanding versus distress before acting.
Lastly, remember to match your facial expressions and body language with your words. If you speak with a cross expression, people may believe that you are scolding them even if you use pleasant words. Use gestures and demonstration to help convey your message.
Assisting with Activities of Daily Living
When assisting with Activities of Daily Living, or ADLs, is handled poorly, it often leads to difficult behaviors. Performing ADLs, such as bathing, feeding, toileting, dressing and grooming, are basic to one’s sense of dignity, autonomy, and mastery. Loss of these abilities can lead to frustration, embarrassment and a sense of inadequacy. Fear and frustration associated with ADLs are the source of most difficult behaviors.  A caregiver’s approach to assisting with ADLs can actually trigger problem behaviors. For these reasons, it is extremely important that caregivers approach assisting with ADLs with understanding, respect, and compassion, as this will go a long way toward preventing behavior difficulties and improving the quality of life for the caregiver and care recipient.
A caregiver’s approach to assisting with ADLs can actually trigger problem behaviors. For these reasons, it is extremely important that caregivers approach assisting with ADLs with understanding, respect, and compassion, as this will go a long way toward preventing behavior difficulties and improving the quality of life for the caregiver and care recipient.
Assisting someone in pleasant, meaningful activities can help prevent difficult behaviors. Activities such as gardening, food preparation, or folding towels and napkins can provide productive and pleasant occupation of energy that might otherwise be channeled to worry and frustration. Dancing and other physical exercise can help to dissipate the energy associated with anger that could otherwise be used for aggression. Remember to modify activities to promote autonomy and increase the likelihood of success.
Click here to read more about assisting with activities of daily living, or ADLs.
Retrogenesis
Research has shown that in dementia, functional abilities are lost in the reverse order that they were gained during childhood and adolescence.
This is called reverse development retrogenesis.
Functions, such as walking, speaking, self feeding, riding a bicycle and driving a car are lost in roughly the reverse order that they were learned from childhood into teenage years.
Understanding this concept is very useful in explaining behaviors and in developing ways to handle the behaviors.
Interventions should be based on learning and functioning at various stages of development. Because most caregivers have raised or helped to raise children, they can see the similarities in behaviors and call upon their own experiences to understand and address the behaviors.
A person in the early stages of dementia loses the functions gained roughly between 7 to 12 years of age. For example, similar to how an 8-year-old child would know how to dress but may not think to put on a coat to go play outdoors in the winter, a person in the middle or even late early stages of dementia might not think to put on a coat in winter either. So towards the end of the early stages of Alzheimer’s, a person may be functionally similar to a 7- to 12-year-old child.
Retrogenesis (Continued)
 A 4- to 5-year-old child may not be able to distinguish a bottle of soda from a bottle of cleaning solution. Someone in the middle stages of Alzheimer’s would not be able to make the same distinction either.
A 4- to 5-year-old child may not be able to distinguish a bottle of soda from a bottle of cleaning solution. Someone in the middle stages of Alzheimer’s would not be able to make the same distinction either.
By the late or terminal stage of Alzheimer’s disease, a person’s functionality is similar to an infant’s. An infant up to the age of 2 years is incontinent or at least not completely in control of bladder and bowel movements, just like a person in the late stages of Alzheimer’s.
When the person with Alzheimer’s is spitting food out, taking food from another person’s plate, or going outdoors barefoot in winter, remember your children doing that when they were little, and think about ways that you handled those situations. Some of the approaches you used on your children may work with adults with Alzheimer’s.
At the same time, caregivers must keep in mind that even though there are similarities in behavior, there are important differences between children and adults.
Even if your approach does not work, at least knowing about reverse development will help you to understand what is going on and may relieve some of your own frustration.
Stress Threshold
One way to try to prevent difficult behaviors is to look for signs that people are approaching their stress threshold and to reduce their stress before it results in agitation behaviors. As dementia progresses, the person becomes  less and less able to cope with stress and so instead, reacts with agitation, combativeness, or other negative behavior. Part of the problem is that as Alzheimer’s disease progresses, the person experiences progressively lowered stress threshold. The person’s tolerance for stress declines so that smaller things can produce a stress response. As individuals become less able to master their environment and the tasks of daily living, they become frustrated, which leads to stress. They are not aware of the increasing stress or of ways to cope with it, so they react in more primitive ways such as lashing out, wandering, pacing, or combativeness.
less and less able to cope with stress and so instead, reacts with agitation, combativeness, or other negative behavior. Part of the problem is that as Alzheimer’s disease progresses, the person experiences progressively lowered stress threshold. The person’s tolerance for stress declines so that smaller things can produce a stress response. As individuals become less able to master their environment and the tasks of daily living, they become frustrated, which leads to stress. They are not aware of the increasing stress or of ways to cope with it, so they react in more primitive ways such as lashing out, wandering, pacing, or combativeness.
The caregiver’s job is to look for signs that people are approaching their stress threshold. These signs include restlessness and pacing, tense facial expressions, irritability, calling out, and scratching or hand wringing.
When people near their stress threshold, caregivers can try to help relieve the stress through exercise, taking a break, or redirecting to relaxing activities. Research has also shown that aromatherapy using essential oil of lemon balm (also known as Melissa oil) or lavender oil can reduce stress and agitation behaviors, particularly when combined with massage therapy. For instance, lemon balm can be applied to the face and arms twice a day. Additionally, playing a person’s preferred music can also reduce stress and agitation.
Understanding the problem of stress and carefully observing people for signs of increasing stress can go a long way towards preventing behavior outbursts and catastrophic reactions.
Click here to learn more about Progressively Lowered Stress Threshold (PLST).
Principles for Managing Aggression
Before discussing specific strategies for managing difficult behaviors, let’s discuss some principles for managing aggressive behaviors.
 Always keep in mind your safety as well as that of others. During aggressive behavior, do not confront the person or try to discuss the behavior. The person with dementia most likely cannot understand or control it.
Always keep in mind your safety as well as that of others. During aggressive behavior, do not confront the person or try to discuss the behavior. The person with dementia most likely cannot understand or control it.
Do not touch the person during the angry outburst. Physical contact can trigger physical violence in agitated people. Give people time and space to be angry by themselves, but watch to make sure they do not cause harm to themselves or others.
Let them play out the aggression until it is safe to approach them. Then approach them using a calm manner.
Although in the past, physical restraints were often used to manage some difficult behaviors, in general, restraints are not the best approach. One type of restraint that has some support if used only occasionally is the chair with a lap-top table. These chairs can be used to prevent a person from getting up or falling during activities and meals. If possible, it is best not to use these chairs routinely as a method to control behavior.
It is important to understand that changing behaviors is never simple, so be patient and try your best.
Strategies for Managing Difficult Behaviors
Now let’s discuss two ways to view problem behaviors and different approaches to modify them. This system will give you a simplified way of deciding how to approach the problems you face.
One way to view difficult behaviors is to broadly categorize them as behavior excesses or behavior deficits. Behavior excesses include yelling, pacing, kicking, or arguing. In other words, behaviors that get attention.
Two interventions for behavior excesses include redirecting and withdrawing attention.
Redirecting means to refocus someone’s attention on a more positive topic  or activity. For example, if someone is arguing or engaging in aggressive behavior with another person, the caregiver could go up to the aggressive person, smile, gently take a hand, address the person by name, and say something like: “Robert, please come with me to the kitchen. I need your help to make cookies.” The caregiver has engaged Robert by smiling and taking his hand, has pleasantly invited him to come with her, and has introduced a positive image: cookies. She has also indicated to Robert that he is needed.
or activity. For example, if someone is arguing or engaging in aggressive behavior with another person, the caregiver could go up to the aggressive person, smile, gently take a hand, address the person by name, and say something like: “Robert, please come with me to the kitchen. I need your help to make cookies.” The caregiver has engaged Robert by smiling and taking his hand, has pleasantly invited him to come with her, and has introduced a positive image: cookies. She has also indicated to Robert that he is needed.
Another good way to redirect someone is to change the environment. Offer to go for a walk or go to another room to listen to music with the person. Ask the person if she or he would like to go to the kitchen for a snack or drink.
Another option is to offer to help solve the issue if the situation is resolvable. The person may be acting out because of an unmet need. Or there may be a conflict or issue between the person and someone else that you may be able to help resolve.
A positive interaction with a caregiver may itself be enough to redirect the person. All people need positive social interactions, and those with dementia are no exception. A meaningful interaction with someone else may help the person calm down and forget their negative feelings.
The caregiver must carefully assess the situation to see what may be causing the behavior and what might be the best intervention.
Strategies for Managing Difficult Behaviors (Continued)
 Withdrawing attention means to ignore the difficult behavior. It does not mean to ignore the person. For example, if a person is swearing or making rude remarks, the caregiver can briefly take attention away from the person who is acting inappropriately. When the swearing stops, the caregiver can once again pay attention to the person who was swearing, but should change the subject to something that is pleasant.
Withdrawing attention means to ignore the difficult behavior. It does not mean to ignore the person. For example, if a person is swearing or making rude remarks, the caregiver can briefly take attention away from the person who is acting inappropriately. When the swearing stops, the caregiver can once again pay attention to the person who was swearing, but should change the subject to something that is pleasant.
The key principle is to reward positive behaviors and show value to the person with attention, and to withdraw attention during negative behavior excesses.
It is similar to a common approach used when a child has a temper tantrum. The approach is to ignore the tantrum, but to give the child attention when not having tantrums. You are ignoring the behavior, but under other circumstances, showing value to the person with attention. The technique of withdrawing can be effective with behaviors that may be offensive to others but are not serious or harmful. It is best not to ignore behaviors that could cause harm to self or others.
Keep in mind that attention and positive interactions should be provided throughout the day. Those with dementia need to know that you are there and that they are valued. They should not have to resort to negative behavior to get your attention or to know that you value them.
Managing Wandering
Wandering can be categorized as a behavior excess. There are several types of wandering. It may be purposeful (with a goal), escapist (which means  the person is trying to get away), aimless (such as pacing), searching (for persons or objects), or modeling (meaning following others).
the person is trying to get away), aimless (such as pacing), searching (for persons or objects), or modeling (meaning following others).
If the wandering if not harmful to the person or to others, it can be a good form of exercise. It can be redirected and managed so that it is safe and enjoyable.
Strategies for managing wandering include:
- Modifying the environment to provide designated safe areas for wandering with adequate lighting and minimal hazards.
- Providing points of interest in areas of wandering that may redirect the person.
- Planning mini-breaks or rest periods. Provide inviting places for the person to sit and relax.
- Providing comfortable, safe shoes.
- Offering regular hydration and trips to the toilet.
- Offering activities or exercise to distract the person from wandering or pacing.
- Making sure the person gets enough regular exercise during the day to relieve any restlessness.
- Providing many meaningful, enjoyable activities during the day to prevent boredom.
- If wandering tends to occur at a particular time of day, distract the person during that time.
- Reduce overstimulation and stressors in the environment, such as noise or clutter.
- Orient and reassure the person if she or he is confused.
- If you are moving the person to a new environment, reduce disorientation by acclimating them ahead of time with several visits with a familiar caregiver.
- If a person is at risk of wandering away from home or the residence, consider placing a locator device or a wanderer alert device on the person and enrolling in the Alzheimer Association’s Safe Return program.
Click here to read more about assisting with activities of daily living, or ADLs.
Managing Rummaging or Gathering
 Rummaging and gathering can be considered a behavior excess. If it is not harming the person or others, let the person do it.
Rummaging and gathering can be considered a behavior excess. If it is not harming the person or others, let the person do it.
Strategies for controlling rummaging include setting up rummaging boxes on a table; designating some drawers in a desk, table, or dresser for rummaging; setting out purses or a briefcase filled with items; and creating a packet of cards, letters, or papers to sort and read. Be sure to exclude any dangerous objects from anywhere the person rummages.
If individuals like to gather or pack things, provide them with a safe place where they can store items. Try offering a canvas bag, purse, small suitcase, box, or a drawer.
Another thing to consider is whether the person is try to solve a problem when rummaging or gathering. If so, perhaps helping the person to find a solution can help resolve the behavior and strengthen the relationship between caregiver and care recipient.
Another option is to redirect the person by providing an activity that the person enjoys doing that uses similar repetitive motions. Examples include sorting yarn or coins, or folding towels.
Behavior Deficits: Apathy and Depression
The other category of challenging behaviors is behavior deficits, such as apathy and depression. When individuals with dementia experience  apathy or depression, they will have more difficulty performing tasks and following what you are saying.
apathy or depression, they will have more difficulty performing tasks and following what you are saying.
Apathy can be a symptom of Alzheimer’s disease, and depression is often seen in those with Alzheimer’s. Apathy and depression are related but are separate conditions. Apathy is a dulled emotional state characterized by indifference. Apathetic people show little or no emotions, may appear bored and uninterested in interacting with others. Apathy can be recognized by the person’s diminished initiative, poor persistence in activities, lack of interest, low social interaction, blunted emotional response and lack of insight. Apathy can be a symptom of depression.
Depression is a mental illness that usually presents with a marked lack of interest, loss of motivation, feelings of hopelessness, fatigue, poor concentration, difficulty making decisions, suicidal thoughts, and low self-esteem.
Both can contribute to withdrawal, immobility, malnourishment, poor dental hygiene and many other debilitating situations that can lead to faster functional and physical decline.
Managing Apathy and Depression
Two approaches for managing behavior deficits are directing and simplifying. Because apathetic or depressed individuals seem to be indifferent to their environment and what is expected of them, it is necessary to be more directive with them and to simplify communication and actions.
What is directing? Directing is a way of engaging people in activities by pointing out what they need to do and encouraging them to participate and respond. It does not mean to stand over them, commanding them to obey. When people are very passive, not involved, or neglecting themselves, they need to be reminded or encouraged to respond. It is necessary to be more directive with them, but in a gentle, respectful way. Using a gentle approach will decrease the odds of provoking a negative reaction. For example, Mary can walk over to Robert, take his hand and say, “Robert, it is time for dinner. I will take you to the dining room. “
 Mealtime takes a good portion of any given day and can be a good opportunity to engage an apathetic or depressed person in a positive experience. To help make it a pleasant occasion, caregivers can eat their meals with their care recipients and try to make it a social event. This means engaging the individuals by sitting down beside them, saying their name, making eye contact, and carrying on a conversation.
Mealtime takes a good portion of any given day and can be a good opportunity to engage an apathetic or depressed person in a positive experience. To help make it a pleasant occasion, caregivers can eat their meals with their care recipients and try to make it a social event. This means engaging the individuals by sitting down beside them, saying their name, making eye contact, and carrying on a conversation.
Simplifying activities can reduce stress and increase the likelihood of success, which can in turn promote self-confidence and esteem. Activities can be adapted to match the level of the person’s capacities and skills by breaking up the activity into simple steps, setting up activities and equipment in ways that the person can manage, shortening activities, and slowing down it’s pace.
Behavior Deficits: Apathy and Depression (Continued)
A good way to help treat apathy and depression is through physical exercise. All people need regular exercise and daily activities that entertain and engage them. Exercise improves respiration and circulation,  increasing the delivery of oxygen & nutrients in the blood to the brain and other organs. Research has shown that exercise improves mental and physical health. So caregivers should encourage people to get regular exercise, such as walking, tossing a ball, and chair exercises. Doing exercises together also allows caregivers to spend quality time with their care recipients and improve their own health.
increasing the delivery of oxygen & nutrients in the blood to the brain and other organs. Research has shown that exercise improves mental and physical health. So caregivers should encourage people to get regular exercise, such as walking, tossing a ball, and chair exercises. Doing exercises together also allows caregivers to spend quality time with their care recipients and improve their own health.
Anyone who has symptoms of apathy or depression should also be evaluated by a healthcare professional. Distinguishing depression from apathy is important, as depression is a serious medical issue often treatable with medications, and if left untreated, can lead to suicide.
Behavior Deficits: Hallucinations, Illusions, and Delusions
People with dementia often experience frightening hallucinations, illusions and delusions, which can trigger difficult behaviors such as physical or verbal aggression. These perceptual distortions are the result of the disease and need to be understood in order to provide the best  care.
care.
A hallucination is the perception of something that is not there. A hallucination can involve any of the senses (sight, hearing, smell, taste, or touch). Seeing something that is not there is called a visual hallucination, and hearing something or someone that is not there is an auditory hallucination. These two types of hallucinations can be experienced together or separately. For example, a person may see and hear a deceased family member.
An illusion is somewhat different from a hallucination. An illusion is the misperception or misinterpretation of an object or person. For example, someone may see a hat rack and misinterpret it as a person. Individuals may see their own image in a mirror or a darkened window and, not recognizing themselves, believe that another person is in the room. All of these false or mis-perceptions are caused by damage to the parts of the brain that process sensory information, so they seem very real to the person experiencing them.
Behavior Deficits: Hallucinations, Illusions & Delusions (Continued)
A delusion is a false idea or belief that is strongly held. For example, Robert may wrongly believe that his wife, Mary is having an affair with the male caregiver who comes to assist with his bathing and dressing. In Alzheimer’s disease, damage to the brain cells and pathways that help make  sense of the world result in fear and confusion, which in turn can lead to suspiciousness and paranoia, particularly at night when familiar clues in the surroundings are shadowed.
sense of the world result in fear and confusion, which in turn can lead to suspiciousness and paranoia, particularly at night when familiar clues in the surroundings are shadowed.
Paranoia describes unwarranted or exaggerated mistrust or suspiciousness of others that causes excessive fear and anxiety. It often involves a sense of persecution and threat towards oneself. Paranoia can reach the point of being a delusion. For example, a woman with dementia may have the fixed belief that her caregiver is trying to poison her in order to take her belongings. The person may refuse to eat because of this or may attack the caregiver.
Even though people with dementia have poor memories, they can retain a strong sense of territory and belongings. Caregivers need to be careful in such situations so as not to give any reason to be suspicious.
Managing Hallucinations, Illusions, and Delusions
When dealing with false perceptions, four general approaches that caregivers should try are to:
Empathize rather than argue or criticize. It is best not to argue with individuals about what they think or believe they see or hear. Hallucinations, illusions, and delusions are very real to the persons experiencing them, and trying to convince them that they are not real will likely lead to frustration and agitation.
 Instead, caregivers should offer reassurance that everyone is safe and everything is okay. To goal is to offer comfort to calm the person. Say something like, “Robert, I do not see a man in the room, but I know it must be scary for you. Don’t worry, I will not let anyone hurt you. You are safe here. I will stay with you for a while.”
Instead, caregivers should offer reassurance that everyone is safe and everything is okay. To goal is to offer comfort to calm the person. Say something like, “Robert, I do not see a man in the room, but I know it must be scary for you. Don’t worry, I will not let anyone hurt you. You are safe here. I will stay with you for a while.”
Then try to find “solutions” with the person to relieve the fear or anxiety. For example, if a woman with dementia believes that her jewelry has been stolen, offer to look for the jewelry with her. If she believes a stranger is in the room, then offer to look around the room to see if anyone is there. If she believes that her son has been hurt in an accident, offer to call him on the telephone with her.
Lastly, try to redirect and provide a new environment. Offer a pleasant activity, go for a walk together, talk about favorite topics such as family, hobbies, or memorabilia, offer a snack or drink, listen to music, or take the person to a new room.
These strategies can be effective with many difficult behaviors. Let’s look at some examples.
Managing Hallucinations, Illusions, and Delusions (Continued)
If someone experiences a hallucination or illusion, caregivers should look for possible causes in the environment. Many older individuals have poor eye sight which can contribute to hallucinations and illusions. Check for things like shadows, mirrors, and uncovered windows that might be causing the misperception. Cover or remove mirrors, and cover windows to prevent reflections and outside lights. Adjust lighting and objects in the room to reduce shadows. Lighting should be bright enough even at night to eliminate dark corners and shadows. The room should be arranged so that large items such as a hat rack will not cause shadows, and clutter removed to prevent confusion and injuries. Hazardous objects should be removed to prevent fear of harm or threat.
If the person believes that someone is in the room, then the caregiver should look around to reassure the person that no one is there. This will acknowledge and respect the person’s assertions and feelings.
 What may seem like auditory hallucinations could be sounds in the environment. For example, paging systems, the television next door, or people conversing within earshot, can be misinterpreted. Investigate for possible real causes of the voices and sounds, and correct them. For example, if the television is on, turn it off and assure the person that it was the TV making all that noise by saying something like, “Robert, it was the TV making all that noise. I will turn it off so that you can have some quiet.”
What may seem like auditory hallucinations could be sounds in the environment. For example, paging systems, the television next door, or people conversing within earshot, can be misinterpreted. Investigate for possible real causes of the voices and sounds, and correct them. For example, if the television is on, turn it off and assure the person that it was the TV making all that noise by saying something like, “Robert, it was the TV making all that noise. I will turn it off so that you can have some quiet.”
If individuals hear frightening voices, and there is no external cause, reassure them that you do not hear the voices and that you will see that no harm will come to them. Try to stay with them for a while, diverting their attention to something pleasant.
It would also be wise to observe them for a while to make sure there is no danger of harm to self or others.
Managing Hallucinations, Illusions, and Delusions (Continued)
Because of the short attention span and memory loss associated with Alzheimer’s disease, one useful strategy for managing false perceptions is to use diversion or redirecting to something pleasant. For instance, reminiscing about old memories or looking at a family photo album can move a person’s attention away from a frightening experience to a pleasant 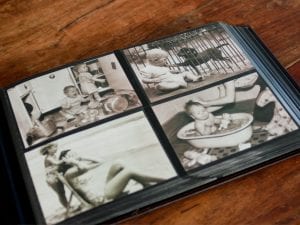 one. Ask the person to tell you about someone in a photo or about past vacations. Another option to change the environment by offering a snack in the kitchen, or listening to music in another room.
one. Ask the person to tell you about someone in a photo or about past vacations. Another option to change the environment by offering a snack in the kitchen, or listening to music in another room.
Delusions and paranoia are not easy to address, as they often are so fixed in the person’s mind. Again, it is helpful not to argue, but rather to reassure the person. For example, saying, “Your husband loves you very much,” or, “She is very proud of you,” can provide some reassurance. Then try redirecting their attention by asking, “How did you two meet?” or, “Will you tell me about your wedding?”
It can be helpful to compliment and build up the person’s self-esteem before providing a diversion. For example, tell the person that she looks lovely or that he looks handsome. If some individuals like to sing, tell them that you think they sing beautifully and ask them to sing a song with you. Or, if applicable, ask them to tell you about their experiences singing in a group or choir. These strategies will promote self-worth and allow people to reminisce about happy times.
Another approach to managing delusions and hallucinations is to consult a healthcare professional about medications or changes to the current medication regimen that may be able to reduce their occurrence. Sometimes changing doses or medication times can help reduce unwanted side effects such as altered perceptions.
ABCs of Behavior Management
Another approach to managing difficult behaviors is called the ABCs of behavior management, which was developed by Dr. Linda Teri. The underlying principle of this method is to change behaviors using two approaches: by modifying things in the environment that may be triggering the behavior or by changing the consequences to the behavior in order to prevent negative reactions, or difficult behaviors.
The “A” in the ABCs of behavior management stands for “Antecedent,” which refers to whatever happened before the behavior occurred. It is  essentially the trigger for the behavior. For example, Robert may have the delusion that his male caregiver is having an affair with Mary. If Mary whispers something in the caregiver’s ear, that could trigger Robert to become angry and act aggressively.
essentially the trigger for the behavior. For example, Robert may have the delusion that his male caregiver is having an affair with Mary. If Mary whispers something in the caregiver’s ear, that could trigger Robert to become angry and act aggressively.
What could be done to modify the antecedent?
Mary should be cautious about having private conversations with others, particularly men, in the presence of her husband. The caregiver could gently refuse to let Mary whisper in his ear, asking her to telephone or speak with him outside instead.
ABCs of Behavior Management (Continued)
The “B” stands for Behavior. In this program, this represents a problem behavior, such as aggression. For example, Robert might hit the caregiver after seeing him talk to Mary. The seeming intimacy of whispering to the caregiver caused Robert to become jealous and respond with physical aggression.
The “C” refers to the Consequence, or what happens after the behavior. In this example, the consequence may be the caregiver avoiding Mary’s close contact in the future in order to prevent upsetting Robert.
The caregiver could also wait until Robert had time to recover, then try to distract him from his jealous worries by sitting down with him and asking about his children, or asking about his hobbies, such as bird watching.
Also, the caregiver could suggest to Mary that she spend some private time  together with Robert to reduce his jealous feelings.
together with Robert to reduce his jealous feelings.
The ABCs of behavior management is a good way to think about behaviors, people, and the environment that might trigger a behavior incident. Sometimes it is necessary to make these observations over time before it becomes clear to you what happens. Take notes about the incidents and discuss things with other caregivers. This can not only be helpful to you but to the others as well.
Click here to learn more about ABC’s of Behavior Management
Medications
A healthcare professional should be consulted if considering medications  for managing difficult behaviors and reducing a person’s level of anxiety and agitation. In general, medications should be prescribed at the minimal effective dose. This means that the dose should relieve the symptoms with as few side effects as possible. In the case of medications for managing agitation and anxiety, the side effect of sedation should be minimized so that the person can still participate in activities.
for managing difficult behaviors and reducing a person’s level of anxiety and agitation. In general, medications should be prescribed at the minimal effective dose. This means that the dose should relieve the symptoms with as few side effects as possible. In the case of medications for managing agitation and anxiety, the side effect of sedation should be minimized so that the person can still participate in activities.
A healthcare professional should also be consulted if there are sudden or significant changes in a person’s behavior or functional abilities. Such changes can be an indication of serious medical issues.
Summary
In summary, some key approaches for managing difficult behaviors include identifying specific behaviors and designing specific interventions, setting appropriate and realistic goals, making ongoing assessments and adjustments, and being willing to try new and creative strategies. Principles for managing difficult behaviors include reducing frustration and fear, providing safety, security and comfort, using good communication techniques, and using person-centered care. Caregivers should try to anticipate needs and address them before they lead to difficult behaviors when possible. Another strategy for preventing difficult behaviors is to look for signs that people are approaching their stress threshold and to relieve their stress before it leads to agitation behaviors.
To manage difficult behaviors, use reassuring words with a smile, gentle tone of voice, and comforting gestures with a non-threatening posture. Effective interventions include music therapy, aromatherapy, exercise, pleasant activities, and meaningful interactions with other people. Another method is to use the ABCs of behavior management, which tries to change behaviors by modifying the antecedent or the consequences to the behavior.
Strategies for managing behavior excesses include redirecting and withdrawing attention, whereas directing, simplifying, and physical exercise may help improve behavior deficits such as apathy and depression. Wandering, pacing, rummaging and gathering may be allowed in safe settings. Hallucinations, illusions, and delusions should be managed with reassurance, environmental modifications and distraction. During an outburst of aggressive behavior, do not try to discuss the behavior or touch the person until it is safe to approach.
A combination of medication and behavior approaches can help reduce many difficult behaviors. But in all cases, non-pharmacological approaches should be attempted.
← Previous Lesson (Difficult Behaviors Associated with Dementia)
→ Next Lesson (Early Stages: Family Involvement and Planning)
. . .
Written by: Catherine M. Harris, PhD, RNCS (University of New Mexico College of Nursing), and Linda Teri, PhD (University of Washington School of Medicine)
Edited by: Mindy J. Kim-Miller, MD, PhD (University of Chicago School of Medicine), and Lena G. Ernst, PhD (University of New Mexico)
References:
- Allen RS, Burgio LD, Fisher SE, Hardin JM, & Shuster JL, (2005). Behavioral characteristics of agitated nursing home residents with dementia at the end of life. The Gerontologist 45: 661-666.
- Bartels SJ, Horn SD, Smout R, Dums AR, et al. Agitation and depression in frail nursing home elderly patients with dementia. (2003). Am J Geriatr Psychiatry 11:231-238.
- Ballard C, O’Brien J, Reichelt K, & Perry E. (2002). Aromatherapy as a safe and effective treatment for the management of agitation in severe dementia: The results of a double-blind, placebo-controlled trail with Melissa. Journal of Clinical Psychiatry, 63: 553-8.
- Beck C, Frank L, Chumbler NR, O’Sullivan P, Vogelpohl TS, Rasin J, Walls R, & Baldwin B, (1998). Correlates of disruptive behavior in severely cognitively impaired nursing home residents. The Gerontologist 38(2): 189-198.
- Boettcher IF, Kemeny B, DeShon RP, & Stevens AB, (2004). A system to develop staff behaviours for person-centred care. Alzheimer’s Care Quarterly 5(3): 188-196.
- Bourgeois, MS & Burgio, LD, (1997). Modifying repetitive verbalizations of community-dwelling patients with AD. The Gerontologist 37(1). 30-40.
- Burgener S, Murrell L, & Shimer R, (1993). Expressions of individuality in cognitively impaired elders: the need for individual assessment and approaches to care.Journal of Gerontological Nursing 19: 13-22).
- Burgio L, (1996). Interventions for the behavioral complications of Alzheimer’s disease: Behavioral approaches. International Psychogeriatrics 8: 45-53. Christine K.Alternatives to restraint use.
About.com. (August 2006). Retrieved on February 24, 2009 from http://alzheimers.about.com/od/practicalcare/a/Restraints_2.htm.
- Cohen-Mansfield, J. (2000). Nonpharmacological management of behavioral problems in persons with dementia: The TREA model. Alzheimer’s Care Quarterly, Fall,1(4), 22-34.
- Cummings, J. (2004). Alzheimer’s disease. The New England Journal of Medicine, 351, 56-67.
- Dettmore, D., Kolanowski, A., & Boustani, M. (2009). Aggression in persons with dementia: Use of nursing theory to guide clinical practice. Geriatric Nursing, 13(1), 8-17.
- Feil, N (1982). Validation: The Feil method. Edward Feil Productions. Cleveland Ohio.
- Hall GR, Buckwalter KC, (1987). Progressively lowered stress threshold: A conceptual model for care of adults with Alzheimer’s disease. Archives of Psychiatric Nursing 1(6): 399-406.
- Hall,GR, GerdnerLA, Zwygart-Stauffacher M, & Buckwalter KC, (1995). Principles of nonpharmacological management: Caring for people with Alzheimer’s disease using a conceptional model. Psychiatric Annals 25(7): 432-440.
- Hay, D., Klein, D., Hay, L., Grossberg, G., & Kennedy, J. (2003). Agitation in patients with dementia. Washington, DC: American Psychiatric Publishing.
- Hellen CR, (2004). Enabling success: Hands-on care strategies and behavioral refocusing interventions. Alzheimer’s Care Quarterly 5(2: 178-182.
- Holmes C, Hopkins V, Hensford D, MacLaughlin V, et al. (2002). Lavender oil as a treatment for agitated behaviour in severe dementia: a placebo controlled study. Int J Geriatr Psychiatry. 17:305-8.
- Kunik ME, Lees E, Snow AL, Cody M, Rapp CG, Molinari VA, & Beck, CK, (2003). Disruptive behavior in dementia. Alzheimer’s Care Quarterly 4(2): 125-136.
- Landes AM, Sperry SD, Strauss ME, & Geldmacher DS, (2001). Apathy in Alzheimer’s disease. Journal of the American Geriatrics Society 49:1700-1707.
- Lin PW, Chan WC, Ng BF, Lam LC. (2007). Efficacy of aromatherapy (Lavandula angustifolia) as an intervention for agitated behaviours in Chinese older persons with dementia: a cross-over randomized trial. Int J Geriatr Psychiatry. 22:405-10.
- Logsdon RG, McCurry SM, Teri L, (2005). A community based approach for teaching family caegivers to use behavioral strategies to reduce affective disturbances in persons with dementia. Alzheimer’s Care Quarterly 6(2) 146-153.
- Logsdon, R., McCurry, S., & Teri, L. (2007). Evidence-based psychological treatments for disruptive behaviors in individuals with dementia. Psychology and Aging,22(1), 28-36.
- Lyketsos, C. (2007). Apathy and agitation: Challenges and future directions. American Journal of Geriatric Psychiatry, 15(5), 361-364.
- Martinio-Salzman, D., (1991). Travel behavior of nursing home residents perceived as wanderers and nonwanderers. Gerontologist. 31(5): 666.
- McCabe BW, Baun MM, Speich D, & Agrawal S, (2002). Resident dog in the Alzheimer’s special care unit. Western Journal of Nursing Research 24(6): 684-696.
- Nagaratnam N, & Gayagay G, (2002). Hypersexuality in nursing care facilities. Archives of Gerontology and Geriatrics 35(3): 195-204.
- Nagaratnam N, Patel L, Whelan C, (2003). Screaming, shrieking and muttering: the noise-makers amongst dementia patients. Archives of Gerontology and Geriatrics 36(3):247-259.
- Neugroschi, J. (2002). How to manage behavior disturbances in the older patient with dementia. Geriatrics, 57(4), 33-37.
- Phillips, V., & Diwan, S. (2003). The incremental effect of dementia-related problem behaviors on the time to nursing home placement in poor, frail, demented older people. The Journal of the American Geriatrics Society, 51, 188-193.
- Ramadan FH, Naughton BJ, Prior R, (2003). Correlates of behavioral disturbances and pattern of psyhchotropic medication use in five skilled nursing facilities. Journal of Geriatric Psychiatry and Neurology 16(1): 8-14.
- Richards K, Lambert C, Beck C, (2000). Deriving interventions for challenging behaviors from the need-driven dementia-compromised behavior model. Alzheimer’s Care Quarterly 1(4): 62.
- Roberts S, Durnbaugh T, (2002). Enhancing nutrition and eating skills in long-term care. Alzheimer’s Care Quarterly 3(4): 316-329.
- Russell D, Barston S, White M. Alzheimer’s behavior management: Learn to manage common behavior problems. (December 2007). Helpguide.org. Retrieved February 26, 2009 from http://www.helpguide.org/elder/alzheimers_behavior_problems.htm.
- Samus, Q., Rosenblatt, A., Steele, C., Baker, A., Harper, M., Brandt, J., Mayer, L., Rabins, P., & Lyketsos, C. (2005). The association of neuropsychiatric symptoms and environment with quality of life in assisted living residents with dementia. Gerontologist, 45(1), 19-26.
- Schneiderman, N., Ironson, G., & Siegel, S. (2005). Stress and health: Psychological, behavioral, and biological determinants. Annual Review of Clinical Psychology, 1,607-628.
- Skjerve A, Holsten F, Aarsland D, Bjorvatn B, Nygaard HA, Johansen I, (2004). Improvement in behavioral symptoms and advance of activity acrophase after shortterm bright light treatment in severe dementia. Psychiatry and Clinical Neurosciences 58: 343-347.
- Snow LA, Hovanec L, Brandt J. (2004). A controlled trial of aromatherapy for agitation in nursing home patients with dementia. J Altern Complement Med. 10:431-7.
- Sung HC, Chang AM. (2005). Use of preferred music to decrease agitated behaviours in older people with dementia: a review of the literature. J Clin Nurs. 13:1133-40.
- Teri, L., Logsdon, R., & McCurry, S. (2002). Nonpharmacologic treatment of behavioral disturbance in dementia. The Medical Clinics of North America, 86, 641-656.
- Teri, L., Logsdon, R., Peskind, E., Raskind, M., Weiner, M., Tractenberg, R., Foster, N., Schneider, L., Sano, M., Whitehouse, P., Tariot, P., Mellow, A., Auchus, A.,Grundman, M., Thomas, R., Schafer, K., & Thal, L. (2000). Treatment of agitation in AD – A randomized, placebo-controlled clinical trial. Neurology, 55, 1271-1277.
- Teri, L., Logsdon, R., Weiner, M., Trimmer, C., Thal, L., Whall, A., Peskind, E., & Members of the Alzheimer’s Disease Cooperative Study. (1998). Treatment for agitation in dementia residents: A behavior management approach. Psychotherapy, 35(4), 436-443.
- Zeisel J, Silverstein NM, Hyde J, Levkoff S, Lawton MP, & Holmes W, (2003). Environmental correlates to behavioral health outcomes in Alzheimer’s special care units.The Gerontologist 43: 697-711.

